Major Depressive Disorder (MDD) is a serious mental health issue diagnosed through professional evaluation using criteria like DSM-5. Advanced depression treatment programs emphasize evidence-based methods, including Cognitive Behavioral Therapy (CBT), Interpersonal Therapy (IPT), and Mindfulness-Based Cognitive Therapy (MBCT). CBT targets negative thought patterns, IPT focuses on relationship issues, and MBCT prevents relapse. Non-medication approaches like psychotherapy, lifestyle adjustments, and meaningful activities are integral to depression treatment programs. Personalized plans consider symptom severity, history, and lifestyle for optimal outcomes.
Major Depressive Disorder (MDD) is a prevalent and debilitating mental health condition, affecting millions worldwide. Understanding MDD involves recognizing its diverse symptoms and seeking proper diagnosis. This article explores effective therapy approaches for managing depression, including evidence-based methods like Cognitive Behavioral Therapy (CBT) and Interpersonal Psychotherapy (IPT). We delve into personalized treatment programs that combine medication, lifestyle changes, and tailored care for optimal results in navigating the path to recovery from MDD.
Understanding Major Depressive Disorder: Symptoms and Diagnosis
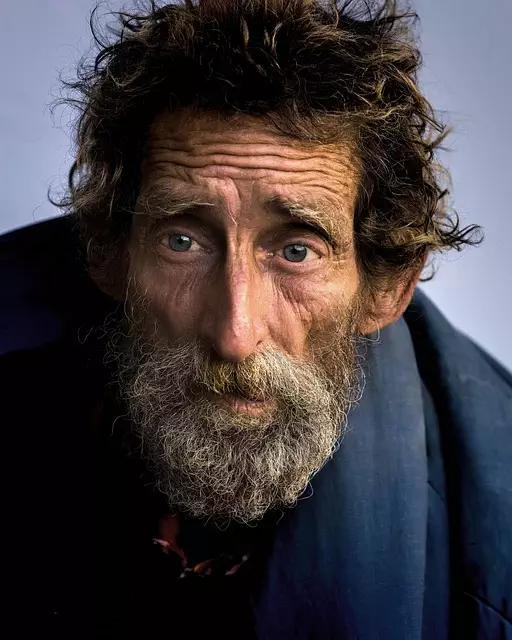
Major Depressive Disorder (MDD) is a common yet severe mental health condition that significantly impacts an individual’s daily life and overall well-being. It goes beyond feeling sad or blue; MDD involves persistent feelings of deep sadness, hopelessness, and loss of interest in activities once enjoyed. Those affected may experience a range of symptoms, including changes in appetite and sleep patterns, fatigue, difficulty concentrating, and recurrent thoughts of death or suicide.
Diagnosing MDD involves a comprehensive evaluation by a qualified healthcare professional. This typically includes a detailed assessment of the individual’s medical history, mental health status, and current symptoms. The diagnosis is made based on specific criteria outlined in diagnostic manuals, such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). A combination of clinical interviews, psychological evaluations, and sometimes additional tests may be used to rule out other conditions and ensure an accurate diagnosis, leading individuals to explore suitable depression treatment programs.
Therapy Approaches for Depression: Exploring Evidence-Based Methods
Depression treatment programs have evolved significantly, with a strong emphasis on evidence-based methods. Cognitive Behavioral Therapy (CBT) is one of the most widely recommended approaches due to its effectiveness in helping individuals identify and change negative thought patterns and behaviors. By focusing on the present and teaching practical coping strategies, CBT empowers patients to manage their symptoms and improve overall well-being.
Another notable therapy approach is Interpersonal Therapy (IPT), which prioritizes understanding and resolving interpersonal issues contributing to depression. This method encourages patients to explore relationships, communicate more effectively, and develop healthier social connections. Additionally, Mindfulness-Based Cognitive Therapy (MBCT) combines elements of CBT with mindfulness practices, such as meditation, to prevent depressive relapses by fostering greater awareness and acceptance of negative thoughts and emotions.
Cognitive Behavioral Therapy (CBT): Unlocking Negative Thought Patterns
Cognitive Behavioral Therapy (CBT) is a highly effective depression treatment program that focuses on identifying and modifying negative thought patterns. This therapy helps individuals challenge and replace distorted beliefs with more realistic, positive ones, thereby improving their emotional well-being. By teaching patients to recognize unhelpful cognitive processes, CBT empowers them to manage depressive symptoms more effectively.
Through structured conversations, therapists guide clients to understand the connection between thoughts, feelings, and behaviors. By doing so, they can help individuals with depression learn to reframe negative thoughts and engage in healthier coping strategies. This process enables people to break free from cycles of negative thinking, which is often at the core of major depressive disorder.
Interpersonal Psychotherapy (IPT): Nurturing Healthy Relationships

Interpersonal Psychotherapy (IPT) is a highly effective depression treatment program that focuses on improving an individual’s relationships and social functioning. This therapeutic approach targets the interpersonal issues that contribute to depression, such as conflicts with loved ones, loneliness, or a lack of social support. By addressing these problems, IPT helps individuals develop healthier relationship patterns and enhances their ability to connect with others.
The core of IPT involves teaching individuals new communication skills to resolve interpersonal difficulties. It encourages patients to express their feelings more effectively, set boundaries, and manage conflicts in a constructive manner. As the individual becomes better equipped to navigate relationships, they often experience a reduction in depressive symptoms and an improved overall well-being. This therapy provides a practical and actionable approach to depression treatment, emphasizing the significant role that social connections play in mental health.
Other Effective Treatments: From Medication to Lifestyle Changes

When considering depression treatment programs, it’s crucial to understand that there are various effective approaches beyond medication. One powerful method is psychotherapy, which includes different types such as cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT). These therapies help individuals identify and change negative thought patterns and improve their relationships.
Lifestyle changes also play a significant role in managing depression. Regular exercise, healthy eating, adequate sleep, and maintaining social connections can significantly enhance mood. Additionally, engaging in activities that bring joy and meaning, such as hobbies or volunteering, can provide a sense of purpose and contribute to overall well-being. Integrating these strategies into a comprehensive depression treatment program often yields more profound and lasting results.
Personalized Depression Treatment Programs: Tailoring Care for Optimal Results

Depression treatment programs are designed to be personalized, recognizing that each individual’s experience with major depressive disorder is unique. Healthcare professionals create tailored care plans that consider factors such as severity of symptoms, personal history, and lifestyle. This individualized approach ensures that treatment strategies align with specific needs, enhancing potential for positive outcomes.
Personalized depression treatment programs may include a combination of psychotherapy, medication management, and lifestyle interventions. For instance, cognitive behavioral therapy (CBT) might be prescribed to help individuals identify and change negative thought patterns. Meanwhile, selective serotonin reuptake inhibitors (SSRIs) could be prescribed for their effectiveness in balancing brain chemicals linked to mood regulation. Additionally, recommendations for regular exercise, mindfulness practices, or support groups complement these evidence-based approaches, fostering holistic recovery.



